If a couple has been waiting for a child for a year, it's a good idea to ask whether there is a medical reason for the wait.
What abnormalities can reduce their fertility?
If a couple has been waiting for a child for a year, it's a good idea to ask whether there is a medical reason for the wait.
What abnormalities can reduce their fertility?
The cause was male in 21% of couples, female in 33% and, in 39% of couples, male and female factors were associated.
For 7 % couples, no explanation was found.
They are very diverse.
Rarely, a man's ejaculation may be physically impaired (e.g. severe diabetes, prostate surgery), but this may be associated with psychological factors.
The spermatozoa present in the semen may be too few in number (oligospermia), too immobile (asthenospermia), or there may be an excess of atypical spermatozoa (teratospermia).
The causes can be found in the pituitary gland, the testicles or the sperm ducts.
It may be a malfunction of the pituitary gland or the testes, due to insufficient secretion.
The testicles may be involved, particularly if, for unknown reasons, they have remained inside the abdomen as they did during foetal life.
Diseases, treatments and certain situations can also affect sperm production: mumps, cancer chemotherapy.
Finally, the presence of varicose veins in the testicles can interfere with spermatogenesis.
Spermatozoa may contain genetic abnormalities, making them unfertile or poorly fertile.
Their production may even be completely stopped, resulting in azoospermia, an exceptional disorder.
Spermatozoa travel through ducts at the exit of the testicles to acquire mobility and be transported outwards.
These may be partially absent since birth, or «blocked» by local infection.
Many products can impair male fertility.
This is certainly true of tobacco, alcohol and drugs.
These days, the environment is a hot topic.
Testicular tissue is very fragile and sensitive to physical agents, such as excessive heat (working in an overheated atmosphere, tight-fitting briefs and jeans that raise testicular temperature), and environmental chemicals, as early as foetal life.
Female causes include tubal abnormalities (32 %), ovulation disorders (30 %), endometriosis (20 %) and recurrent miscarriage (2 to 5 %).
In almost 10 % of cases, the workup is normal and no cause is found.
Age is a very specific factor in the decline of female fertility.
From the age of 30 onwards, female fertility begins to decline and the miscarriage rate rises.
While the average time to conceive between the ages of 20 and 30 is six months, it is gradually increasing.
Fertility declines sharply from the age of 37.
The absence of ovulation, or ovulation of poor quality, can have various origins: it may be a disorder in the control of ovulation by the pituitary gland and the hypothalamus, a disorder in the functioning of the ovaries or, more rarely, the adrenal glands.
When a tube is infected by a disease, particularly a sexually transmitted infection, it closes.
If the disease is bilateral, fertilization becomes impossible, as the spermatozoa can no longer reach the egg waiting at the end of the tube just after ovulation.
It's also a factor in ectopic pregnancy.
Endometriosis is a very special disease.
Its mechanism is still poorly understood.
Menstrual blood contains cells from the uterine lining.
However, these cells sometimes migrate outside the uterus, to the fallopian tubes, ovaries or abdominal cavity.
There, they graft and organize themselves into microcysts.
As these cells are hormone-dependent, they follow the ovarian cycle, causing a small amount of bleeding inside the micro-cyst.
This can lead to pain and adhesions around the uterus.
The meeting between the egg and a spermatozoon becomes difficult.
Uterine causes involve either the cervix or the uterine cavity itself.
After cervical surgery, fertility may be reduced.
Most often, these are abnormalities of the cervical secretion known as «mucus» or «cervical mucus».
It is necessary for the reception of spermatozoa during the conjugal union.
Its role is essential for sperm penetration, storage and subsequent fertilization.
Malformations of the uterus may be involved.
Recurrent miscarriages can be linked to uterine malformations or immune causes.
Tobacco has a recognized and significant harmful effect.
In women who smoke ten cigarettes a day, it takes about twice as long to conceive.
The miscarriage rate is higher, and smoking has harmful effects on the embryo.
Obesity and thinness are factors in hypofertility.
Exposure to a number of chemicals is mentioned, but here too, investigations are needed.
In almost 7 % of cases, the medical check-up finds no explanation.
This is known as functional infertility.
We're all familiar with couples who become pregnant after an adoption, after having given the doctors the cold shoulder, or simply after having considered, not without some pain, that they won't have a child, turning to other projects!
Ultrasound, hormone test, spermogram... several tests are recommended as part of an infertility work-up.
More or less invasive, these tests concern both men and women.

It can be used to detect ovulation disorders.
In practical terms, this means recording your temperature at the same time every morning.
A normal curve shows variations of a few tenths (2 at least): at the start of the cycle the temperature is low, then plummets on the day of ovulation and rises above 37 in the second part of the cycle after ovulation.
It then remains stable, but at a higher level than at the start of the cycle, until the arrival of menstruation.
Find out more about the temperature curve.
This is one of the first procedures requested by the doctor.
Pelvic ultrasound can detect certain ovarian malformations (cysts, etc.) and uterine malformations (fibroids, polyps, malformations, endometriosis, etc.).
In case of suspicion, more detailed tests are prescribed.
Infertility problems can be linked to hormonal disorders.
It is therefore essential to measure certain hormones in the blood to verify their presence and quantity.
We measure levels of estradiol (which stimulates the growth of a follicle under the effect of FSH), FSH (which allows the maturation of a follicle each month), LH (which provokes ovulation), progesterone (a sign of good ovarian function), prolactin (an excess of which disrupts ovulation) and sometimes inhibin B and anti-mullerian hormone (which provide additional information on ovarian reserve, reflecting the age of the ovaries).
It is important to carry out these tests at the right time in the menstrual cycle.
This is an analysis of semen obtained after masturbation at the laboratory.
Sperm motility can thus be observed and counted.
Sperm normally contains between 20 and 400 million spermatozoa. If there are fewer, it's called oligospermia.
Azoospermia is the absence of spermatozoa.
Finally, asthenospermia indicates not the number of gametes, but their low mobility, which is essential to reach and fertilize the oocyte.
If the spermogram shows any «defects», it is advisable to repeat it two or three months later.
This is a vaginal swab, to be taken in the laboratory within hours of sexual intercourse.
The behavior of spermatozoa in cervical mucus is examined.
We can also analyze the mucus, its texture and quantity, which are essential for fertility.
However, this test does not replace a spermogram.
This is an X-ray examination using an opacifying product to see if the fallopian tubes are blocked.
This examination also provides a good view of the uterus.
Several images are usually taken.
The results are immediate.
In very rare forms of male infertility, there is a disturbance of the hypothalamo-pituitary axis.
The equivalent of the pituitary hormones FSH and LH are prescribed, with good results.
They are administered as intramuscular injections every two or three days for four to six months.
Hormones may also be prescribed to restore testicular function.
In other forms of infertility, results are often uncertain, but hormonal treatment can be undertaken to improve sperm quality, possibly before artificial fertilization.
Prostate infections (prostatitis) and sexually transmitted diseases (STDs) must be treated with antibiotics, which are prescribed for a minimum of one month.
Corticosteroids can be beneficial in overcoming the antibodies produced by men against their own sperm.
If the spermogram is not significant and does not show any serious abnormalities, the doctor will look at the patient's lifestyle and suggest :
> Lead a regular, fit lifestyle
> Avoid heat in the testicles: hot baths, tight briefs or pants. For the record, heated briefs have been considered as a contraceptive.
In fact, spermatogenesis is optimal when testicular temperature is just over 37°.
> Beware of sports such as horse riding and cycling. By creating microtrauma, they could exacerbate the problem of hypofertile men.
> Avoid tobacco, coffee, alcohol and overwork.
> Make love often, without falling into an intensive rhythm that could «tire out» the sperm and the couple.
As early as childhood, some young boys undergo surgery when their testicles have remained abnormally in the abdominal position during foetal life, instead of descending towards the bursa.
This condition needs to be operated on, as it may not only impair the future fertility of these children, but above all promote the development of testicular cancer.
In the presence of dilated testicular veins (varicocele), surgical treatment consists in ligating or obturating these veins.
Cet acte chirurgical rétablit la fécondité dans 30 à 50%des cas.
But beware: 20% of men, fertile or not, have a varicocele which, most of the time, poses no fertility problem.
Surgery can restore the permeability of the genital tract.
Permeability corresponds to the passage of gametes into the genital tract.
Even if it is obtained in 30 to 60% of cases, this does not mean a return to fertility.
Many of these men also have abnormal sperm production.
Today, most andrologists - doctors specializing in the male reproductive system - prefer to collect sperm from the epididymides right from the start, with a view to medically assisted procreation.
The surgeon can perform the repermeabilization procedure at the same time as the sperm retrieval.
Infertility problems in women may call for surgery as part of a work-up or to treat a specific cause.
Two techniques are preferred: hysteroscopy and laparoscopy.
Diagnostic hysteroscopy is used to check the uterine cavity and to take biopsies.
It can be used to remove a polyp that is obstructing the implantation of an egg, to lift a septum or to sever an adhesion (synechia).
It allows precise observation of the entire female reproductive system.
During a diagnostic laparoscopy, the surgeon injects a blue-colored product into the uterus via the natural route.
The exit of this product through the end of the fallopian tubes into the abdomen is a sign of their permeability.
For patients with micropolycystic ovary syndrome, this laparoscopic technique involves micro-perforations of the ovaries to induce ovulation.
Between 5 and 10 perforations 5 to 10 mm deep are required.
In the event of infection (such as appendicitis complicated by peritonitis), there is a risk of germs spreading throughout the abdomen.
The body defends itself by building «firewalls» (adhesions) between the various organs.
Other circumstances, such as endometriosis, are conducive to adhesions.
These partitions can prevent the sperm from meeting the egg.
The release of these adhesions and the use of anti-adhesive products in the abdomen attempt to remedy the situation.
This gesture opens the end of a blocked tube.
The surgeon creates a new auricle at the end of a blocked tube containing a clear liquid (hydrosalpinx).
Removal of diseased tubes is sometimes proposed to increase the chances of IVF.
This procedure, which makes a tube permeable after tubal sterilization, is only possible under certain conditions.
Success is variable, with an increased risk of ectopic pregnancy.
In some cases, a fibroid can interfere with implantation or the development of a pregnancy.
Before proposing this procedure, the relationship between the presence of a fibroid and infertility must be ascertained.
Myomectomy refers to the removal of the fibroid.
Endometriosis can cause infertility.
Laparoscopy enables precise mapping of lesions, taking samples, destroying lesions by burning them, removing diseased tissue, reducing pain and improving fertility.
Men also have breasts, but they are less developed than those of women.
Male breast cancer is rare. Less than 1 % of all breast cancers occur in men.
However, it's important for men to be aware that they may be affected by this cancer, particularly so as not to neglect the symptoms.
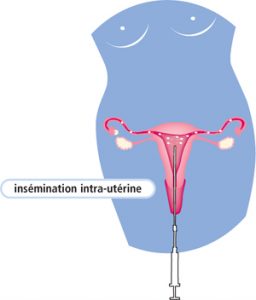
Artificial insemination is performed at an appropriate time in the cycle.
If the cycle is spontaneous, the time of ovulation is determined by the LH peak.
When the cycle is stimulated, ovulation is determined by intramuscular injection of the hormone HCG.
Insemination takes place between 24 and 48 hours after the LH peak or after HCG hormone induction.
It can be performed with fresh or frozen sperm from the partner.
Intrauterine insemination is widely used, enabling one couple in three to avoid the need for more invasive techniques.
The pregnancy rate obtained after one cycle is 15 to 20%.
After 4 to 6 unsuccessful cycles, another reproductive aid such as in vitro fertilization may be proposed.
This technique involves placing spermatozoa and oocytes outside the female genital tract in a culture medium conducive to their survival in the laboratory.
The aim is to fertilize and develop embryos outside the body, hence the term in vitro.
It is intended for women whose fallopian tubes are impermeable, or in the event of failure of other methods, notably 4 to 6 artificial inseminations, or for women over the age of 38.
A number of steps are necessary for proper driving:
Success depends on the quality and number of oocytes collected.
To encourage the development of ovarian follicles and obtain several oocytes, stimulation begins with the daily administration of gonadotropins.
The dose is set by the doctor according to a number of parameters (age, weight, hormonal profile, ultrasound count of antral follicles, etc.).
Follicular maturation lasts an average of 12 days.
As the number and speed of follicle development cannot be predicted, medical supervision is essential after a few days of injections.
It includes regular hormonal blood tests and ultrasound scans.
This is the most important part of the treatment.
Once the follicles are mature (> 17 mm), treatment is stopped. .
An injection of hCG (Pregnyl®) or LH (Ovitrelle®) will artificially induce the final reaction required for ovulation.
This injection must be made at a precise time, always in the evening, so that the eggs can be retrieved just before they leave the follicles, i.e. the morning after the injection.

The oocyte sample is taken 34 to 36 hours after the injection of Pregnyl® (or Ovitrelle®).
The egg has now reached final maturity and is located in the follicular fluid, which can be easily aspirated.
Aspiration is performed via a needle introduced trans-vaginally, under ultrasound control and under general anesthesia, sedation or local anesthesia, in the operating room.
The follicular fluid collected is immediately sent to biologists in the IVF laboratory to isolate the egg it contains.
The number of eggs obtained varies widely. On average, about ten are harvested.
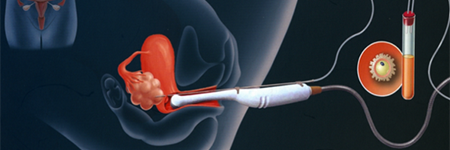
At the same time, on the day of the puncture, the partner must go to the laboratory to collect his sperm. This collection takes place after an abstinence period of around three days. Sperm can also be frozen.
In some cases, a testicular biopsy or aspiration of sperm from the excretory ducts will be required. This is performed before (frozen sperm) or on the same day (fresh sperm) as the oocyte retrieval, under general or local anaesthetic.
Fertilization will be carried out using conventional IVF techniques or microinjection of spermatozoa:
Mature eggs and »hard-working» spermatozoa are collected in a biological culture medium that favors their survival, then stored in a 37° incubator.
A sperm microinjection is performed:
This technique is called ICSI (Intra Cytoplasmic Sperm Injection).
This involves introducing a single spermatozoon into the cytoplasm of the oocyte, under microscopic control using a high-precision device (micro-manipulator).
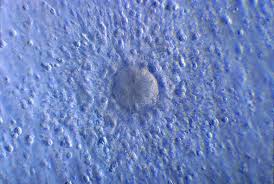
24 hours after fertilization, when the oocyte takes on the appearance of a cell containing two nuclei, the maternal and paternal, fertilization has taken place.
This stage is called2 PN for «two pronuclei».
Fertilized eggs are returned to the incubator and checked under the microscope.
48 hours later, if the fertilized eggs have completed their first cell division, they develop into embryos.
To promote implantation in the uterine mucosa, it is possible to prolong in vitro embryo development.
They are then placed in an environment that provides them with the nutrients they need to thrive.
Embryos can be transplanted between days 5 and 7 of culture, or frozen for later transfer.
This is the moment when the embryo leaves the test tube to enter the mother's womb.
It's a precious moment, like coming to make a promise.
It usually takes place two or three days after the puncture.
The egg or eggs are placed in a very fine catheter which is inserted into the uterine cavity.
The procedure is quick, painless and sometimes followed by hormonal treatment.
The woman can return to work in the days that follow.
That's what everyone's hoping for.
This period is charged with a mixture of hope and anxiety.
After having been in constant contact with the medical profession, the couple found themselves left to their own devices.
A BHCG hormone assay, carried out from day 12 of the transfer, indicates whether or not there is a pregnancy.
If positive, it is checked to confirm the pregnancy.

Dr Nadia Oukacha puts her expertise in gynecology, obstetrics and fertility at the service of every woman, combining listening, prevention and cutting-edge technology.
Each consultation begins with an in-depth discussion to understand your needs and establish a climate of trust.
A complete check-up, nutritional advice and psychological follow-up are adapted to your age and life situation.
Regular smear tests, screening and check-ups aim to anticipate risks and preserve your health over the long term.
Here you'll find answers to the most frequently asked questions about consultations, specialties, booking appointments and how the practice works.
You can book your consultation directly online via our website or by calling the practice on +212 606 12 12 13. A contact form is also available on the site.
Dr Oukacha specializes in :
Gynecology (consultations, pap smears, colposcopy, ultrasounds)
Obstetrics (pregnancy monitoring, ultrasound, amniocentesis)
Intimate and breast surgery
Fertility and medically assisted reproduction (MAP)
The practice is equipped for :
Gynecological and obstetrical ultrasounds
Cervico-vaginal smear
Colposcopy
Fertility assessment
Monday to Friday: 9:00 am - 5:00 pm
Saturday: 9:00 am - 1:00 pm
Sundays and public holidays: closed
The office is located in Casablanca, at 125 BD Brahim Roudani, 1st floor, Appt 11. An interactive map is available on the Contact page.
Access specialized gynecology, obstetrics and fertility care with confidence and simplicity.